Human-Computer Interaction for Older Adults - a Literature Review on Technology Acceptance of eHealth Systems
Journal of Engineering Research and Sciences, Volume 1, Issue 4, Page # 119-126, 2022; DOI: 10.55708/js0104014
Keywords: eHealth, Human-Computer Interaction, HCI, Older adults, Ageing well, Independent living
(This article belongs to the Special Issue on SP1 (Special Issue on Multidisciplinary Sciences and Advanced Technology 2022) and the Section Medical Informatics (MDI))
Export Citations
Cite
Ahmad, A. and Mozelius, P. (2022). Human-Computer Interaction for Older Adults - a Literature Review on Technology Acceptance of eHealth Systems. Journal of Engineering Research and Sciences, 1(4), 119–126. https://doi.org/10.55708/js0104014
Awais Ahmad and Peter Mozelius. "Human-Computer Interaction for Older Adults - a Literature Review on Technology Acceptance of eHealth Systems." Journal of Engineering Research and Sciences 1, no. 4 (April 2022): 119–126. https://doi.org/10.55708/js0104014
A. Ahmad and P. Mozelius, "Human-Computer Interaction for Older Adults - a Literature Review on Technology Acceptance of eHealth Systems," Journal of Engineering Research and Sciences, vol. 1, no. 4, pp. 119–126, Apr. 2022, doi: 10.55708/js0104014.
The population of older adults globally increased during the last couple of decades. Due to these demographic changes, the need for medical care has also significantly increased. Despite the age-related disabilities and chronic diseases, most older adults prefer independent living in their home environment. Technology-enhanced systems and eHealth applications seem to provide some promising solutions for older adults’ well-being and independent living. However, the adoption and acceptance of these applications for older adults are unclear and further research is needed in this area. This study was carried out as a literature review, to meet the aim of identifying and discussing important factors in the Human-computer interaction of eHealth for older adults. The overall research question for this study was: What are the critical factors to consider for an improved human-computer interaction in technology-enhanced health care systems for older adults? Findings indicate some important factors to address: personal integrity, trust, technology acceptance, accessibility of ICT and eHealth literacy. If the presented factors are considered and addressed, it would be easier to achieve the desired aim of independent living. The authors recommend a human-computer interaction that is older adults centred, with the involvement of older adults users in the design process. Proper education and training on the use of eHealth services are also of great importance. Finally, the technology-enhanced system should also provide good social and technological support to the users.
1. Introduction
In most parts of the world, the percentage of older adults increases rapidly, where the fastest growth can be identified in low- and middle-income countries [1, 2]. Today there are globally between 5-600 million people that are 65 years or older, with an estimated increase to around 1.5 billion by the year 2050 [3]. The older people get, the more they will be dependent on medical and social care. In the contemporary society, many older adults are living alone without any support from friends and family members [4].
There are a number of different terms used for the idea of older adults’ right to stay healthy, and to have a rich and joyful life. Some of the most frequently used are successful ageing, active ageing, healthy ageing, positive ageing, productive ageing, competent ageing, and ageing well. These terms have often been combined with the concept of independent living, and the aim of a more cost-effective healthcare [5]. In a strive for consistency, this study has used the terms ageing well and independent living.
The rapid technological development in the 21st century has opened up many new opportunities for eHealth and home care. However, as highlighted by [6], new technology also creates new challenges and critical factors for user acceptance among older adults. Facilitated by an improved human-computer interaction (HCI), eHealth could offer a promising enhancement to traditional healthcare when the percentage of older adults further increases. This study, which builds on our earlier publication [7], has kept the same focus on investigating research studies on eHealth and their findings regarding critical HCI factors for older adults.
The aim of the study was to identify, analyse and discuss important factors in human computer interaction of eHealth for older adults. The overall research question to answer was: What are the critical factors to consider for an improved human computer interaction in technology enhanced health care systems for older adults? For the more long-term objective, the results in this study could hopefully be used as a checklist in the development of eHealth services for older adults.
2. Ageing Well
As found in the large scale cross-sectional study by [8], older adults are concerned about how to age well. In a survey, respondents were asked if they ever had thought about ageing well, and whether their thoughts about ageing well had changed during the previous 20 years. In this respondent group where all persons were aged above 65 years, 90 % had previously thought about ageing well, and about 60% of the respondents said that their thoughts had changed during the previous 20 years. The conclusion of the study was that ageing well is a complex matter encompassing not only physical and functional health, but also psychological and social health [8].
Growing old involves multiple chronic diseases and age-related changes, where endocrine, inflammatory or immune, cardiovascular, and neuroanatomical factors also can cause depression. Late life depressions can have severe consequences, but in general depressions are less prevalent among older adults than what is the case for younger adults [9]. Furthermore, older adults’ social isolation caused by living alone, having small social networks, and infrequent participation in social activities have also been identified as severe health risks [10].
Considering the rapid growth of older adults, several research studies have emphasised the importance of developing new user-friendly eHealth services to support the idea of ageing well [11]. Some recent research articles have pointed out that most older adults prefer to age in their home environments [12]. However, the involved contextual and psychosocial factors must be thoroughly investigated if the new e-health services should be successful, and add value for the well-being of older adults [13,14].
3. Method
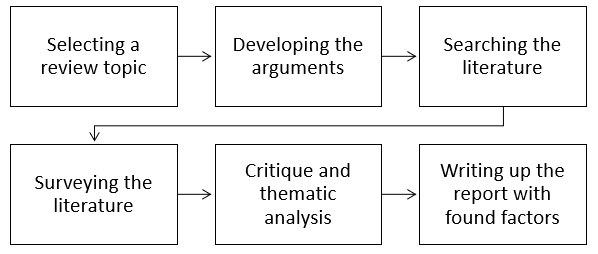
The study design is inspired by the six-step method for literature reviews that has been outlined by [15]. The six ingoing steps are: 1. Selecting a review topic, 2. Developing the tools of argumentation, 3. Searching for literature, 4. Surveying the literature, 5. Critique and analysis of the found literature, and finally 6. Writing up the review with a presentation of results. The first step was carried out during intermissions of a seminar on eHealth, and the second step was a brainstorm session with ideas jotted down on a whiteboard. Step 3 to 6 were carried out iteratively including backward searches on interesting and relevant references in the found articles. In [16], the authors described the term backward search as “reviewing older literature cited in the articles yielded from the keyword search”.
To investigate the current state of Interaction design and HCI for older adults in the area of eHealth, Boolean searches were carried out, using different combinations of the keywords: ‘Human Computer Interaction’, ‘HCI’, ‘eHealth’, ‘eServices’, and ‘Older adults’. The databases for the searches were and Google scholar and Scopus, and with a focus on articles published after 2010. However, some older articles were included when they had findings that could contribute to answer the research question [7]. Furthermore, in this new updated version the earlier result set has been updated with some relevant and more recent publications.
In the first search, with combinations of the keywords above, 456 articles were retrieved. Then authors conducted a screening and read all the article abstracts, with the result that 225 articles were excluded. The common denominator for exclusion was that the articles did not have a direct relationship to the aim and the research question. Later, the remaining 231 articles were further scrutinised to find out if they had a potential to answer the research question. 208 articles were classified as non-relevant and excluded in this step. The remaining 22 articles from the original search were then further categorised into primary articles and secondary articles. The criterion for a primary article is that it must address all important keywords, while a secondary article does not need to contain all the keywords. However, a secondary article had to contain specific and detailed information that would contribute to meet the research aim.
As a part of step 5 in the literature review, results have been thematically analysed and grouped with the aim of finding interesting themes to answer the research question, and to inspire future research. The thematic analysis was conducted as outlined in the article by [17] following the six phases that are listed in Table 1 below.
The first step in this process had the recommended focus of familiarising with the data [17], This immersion process was carried out by reading and rereading the retrieved articles and at the same time taking notes for the further analysis, and to get ideas for the initial coding. Step two involved the start of the systematic analysis, and the initial coding. In [18], the authors have illustrated a thematic analysis as “a brick-built house with a tile roof, your themes are the walls and roof and your codes are the individual bricks and tiles”.
Table 1: The six phases of the thematic analysis
Phase 1 | Articles were read and reread while taking notes |
Phase 2 | Initial codes were generated in the selected articles |
Phase 3 | Codes were collated into preliminary themes |
Phase 4 | Themes were reviewed and cross-checked |
Phase 5 | Definitions and names were generated for all themes |
Phase 6 | Writing up the analytic narrative with found themes |
In the next third step, the code bricks were aggregated into preliminary wall elements, with the idea of capturing “something important about the data in relation to the research question, and represents some level of patterned response or meaning within the data set” [17]. The following fourth involved the recommended quality checking, where the found codes and elements were checked for consistency, and for their potential to contribute to answer the research question. For this fourth step, [18] have facilitating five control questions to support the process:
- Is this an element, a category, or just a code?
- If it is an element or a category, what is the quality of this element or category?
- What are the boundaries of the element or category?
- Are there enough meaningful data to support this element or category?
- Is the element or category coherent?
When the elements and themes or categories were checked, the fifth step handled the definition and naming of the themes. Finally, the sixth remaining step was to write up the presentation of the findings in the thematic analysis, a presentation that can be found below under ‘Results and discussions’.
4. Selected Publications
Table 2 here below shows a chronological listing of the set of selected publications, with information about author(s), study location, and the column for the main study: findings and critical factors. The objective was to provide an up-to-date analysis of Interaction design and HCI in the area of eHealth services for older adults, which in this new version has been updated. At the same time, several relevant and interesting older articles were retrieved in the direct searches, and in the complementary backward searches.
Table 2: Primarily articles in the literature review
Authors | Location | Findings/factors |
Henkemans et al. [19] | Netherlands United States | Visual sensing devices, video monitoring, Ethical considerations, Privacy, Sense of false confidence |
Jung & Loria [20] | Sweden | Compatibility with citizen needs, User’s trust in service provider |
Rogers & Fisk [21] | United States | Understanding older adultism’s needs, preferences, and desires for technology in their lives |
Stojmenova et al. [22] | Slovenia | Technological experience, Education level, Lifestyle characteristics, Cognitive changes, Sensory processes |
Lee & Coughlin [23] | Global- Literature review | Confidence, Emotion, Technical and social support, Affordability, Usability, Usefulness |
Fischer et al. [24] | Global- Literature review | Privacy vs. Utility, Trust, Internet access, Assistive Technology |
Vines et al. [25] | United Kingdom | Embracing alternative measures of success. An HCI research agenda shaped by older people |
de Veer et al. [26] | Netherlands | Awareness, Internet skills, The role of social influence, Ease of use |
Peek et al. [12] | Netherlands | Independent living, behavioural options, personal thoughts on technology use, influence of the social network, influence of organisations and the role of the physical environment |
Axelsson & Wikman [13] | Sweden | Independence was critical among older adults in the sense of control and choice, when older persons use e-health services. |
Ahmad et al. [27] | Sweden | Due to lack of IT literacy and experience, older adults have less acceptance of eHealth applications |
Ma et al. [28] | Malaysia | Social influence, trust, familiarly of a given technology are the main factors of technology acceptance. |
Bong et al. [29] | Norway | Older adults’ participation and involvement in design of digital games is critical for technology acceptance. |
In Table 2, all the listed articles have a direct relationship to both the aim and the research question, which qualify them to be ‘primarily’. Many articles were found irrelevant for this study and excluded, but articles containing interesting details, or with an indirect relation, have been included in the analysis to get more details and to add nuances to the discussion. These ‘secondary articles’ have been listed separately below in Table 3.
Table 3: Secondary articles in the literature review
Authors | Location | Findings/factors |
Rudd et al.[30] | United States | Patient Prospective, Cognitive changes affect the ability to use technology |
Courtney et al. [31] | United States | Self-perception of health, physical condition, mental and emotional condition, anticipatory living, environmental influences, the perceived redundancy of the technology |
Charness & Boot [32] | United States | Attitudinal barriers, Cognitive barriers, Privacy concerns, Age-related changes affecting technology use |
Wagner et al. [33] | Canada | The impact of Person on Environment and the impact of Environment on Person. |
Heart et al. [34] | Israel | Perceived usefulness, perceived impact, Perceived ease of use, Technological issues, Personal traits, Social issues, Facilitating issues |
Xie et al. [35] | United States | e-health literacy and participatory design |
Young et al. [36] | United States | Technological discomfort, Home-based health information technology, electronic health records, data security and confidentiality, |
Latulipe et al. [37] | Korea | Behavioural intention, Data security and accuracy, Socio-Technological environment |
Christophorou et al. [11] | Cyprus | Usefulness, satisfaction and motivation |
5. Findings and Discussions
This study had the aim of identifying, analysing and discussing determinant HCI factors in eHealth services for older adults.
An important main finding in the analysis was the identification of independent living as an overall key concept in designing eHealth systems for older papulation. Many of the selected studies have emphasised the importance of considering older adults’ independence [12, 13, 9, 38, 39]. Independent living is the suggested overall umbrella concept that also has a relation to the other identified factors. In order to accomplish this independence, older adults must have a genuine control over their eHealth services [27, 29, 37, 39, 40]. Moreover, older adults using eHealth services have expressed that activities such as, voluntary work and hobbies are significant determinants of independent living [12]. Figure 2 illustrates the main critical factors that may affect older adults’ independent living.
Other identified factors that support independent living are to facilitate socialisation, communication, and to consider eHealth user’s safety [2, 11, 41]. The study by [13], recommends that eHealth services should be implemented with the aim to strengthen older adults’ mobility and self-management. Moreover, the analysis in this study identified independent living as the major aim for eHealth design for the elderly population. However, in the successful implementation of eHealth services, all the critical factors that are listed below have to be considered.
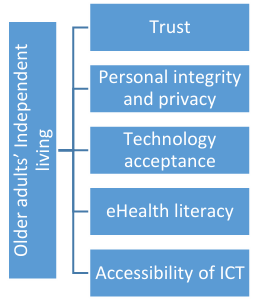
5.1. Trust
Findings clearly show that various forms of trust are a critical factor in HCI design for eHealth systems for older adults. One major factor is users’ trust in the eHealth service providers. eHealth has some identified problems such as the misinterpretation of provided information, technical difficulties, and security and privacy issues. For these matters, the users’ trust in the service provider has been pointed out as the main factor in several studies [20, 42]. Older adults’ confidence in the interaction with high‐technology devices seems to be generally lower if compared to younger people [43]. There are for various reasons a need for support, and a support that includes both technical and social aspects [23]. Trust was also established as a crucial factor in another study on eHealth systems in rural Bangladesh [44].
5.2. Personal integrity and privacy
As discussed in the study by [19], the perceived benefits of using eHealth interventions must be weighed against the perceived privacy concerns. The recommendation from this study is to minimise duration of monitoring technologies, and to never use more monitoring than the actual needs. As an example, a so-called point light camera can transmit images where activities can be distinguished without revealing any personal identity. This can be compared to the more detailed images captured with a video camera, where personal integrity definitely is an issue [19]. Not a surprising finding, but it has been pointed out that users are more willing to use the relatively non-intruding monitoring systems [39].
On the other hand, when the usefulness of eHealth services is perceived as high, users are willing to compromise on privacy. This is an important balance to handle for healthcare providers, the one between the implementation of monitoring systems, and older adults’ privacy [31]. Without respect for personal integrity, the aim of independent living will never be achieved.
5.3. Technology acceptance
Older adults’ attitudes towards the use of eHealth services are strongly dependent on the services’ usefulness, the ease of use, and the general attitude toward using eHealth services [20, 24, 45]. This is not surprising since these are the major factors in the technology acceptance model (TAM). This study also found that the TAM model did not include the dependencies on the quality of internet connection, and on adequate information. The conclusion from the study on technology acceptance carried out by [19], is close to what was discussed in the previous section on trust. Older adults can definitely perceive the benefits of technology in their homes, but the acceptance is related to integrity issues related to monitoring technologies.
The older standpoint that the adoption of technology among older adults mainly is a matter of only costs and performance efficiency has been revised. In [23], the authors highlighted technology acceptance should be seen as a complex issue that is affected by several other factors. Other than usefulness and usability, the most important identified factors were support, emotion, independence, affordability, accessibility, experience and confidence. Regarding the more general eHealth services, a known hypothesis is the preparedness to use eHealth services is increasing for users with high level of ICT proficiency, however, a study by [46] determined that a better ICT experience might increase the intention to use the eHealth services. An explanation might be that older adults with a higher ICT proficiency, also have a good understanding in the risks involved in using eHealth services.
5.4. eHealth literacy
To design user-friendly and inclusive eHealth servises and systems, it is of utmost importance to understand the deficits that come with ageing. eHealth services must be easy to learn and use also for the target group of older adults [25, 47, 48]. However, even with an older adult centred design, eHealth services will hardly be self-explanatory and eHealth literacy is also dependent on proper training [35, 47]. The recommendation from the study by [32], is that the training initiatives for ageing adults ought to consider the age-related changes in ability in the target group.
As brought up by many researchers in the field, an improved education with proper training is considered a fundamental factor for successful eServices for older adults [49, 50]. In an extension of this fundament, the author in study [30] had the remark that education and training is not enough even for adults that have graduated from high school. Furthermore, this study also suggested that new and modern technology such as touch screens and voice activation could be involved to facilitate older adults’ use of eHealth services [30].
In the study [51], the authors observed that ageing has a direct relationship to the ability of understanding information. Older adults often have a reduced ability to use eHealth services and a generally low eHealth literacy. The presented recommendation in the study is to redesign eHealth systems, and that the related eHealth literacy issue should be addressed [51].
Relevant education with a pre-training that involves exercises related to the actual eHealth applications, would certainly improve older adults’ intention and ability to use them. What also seems to be a plausible prediction is that the future will have a growing number of older adults who have used internet services on a regular basis. Persons that have started to use eServices early in life, will probably continue to use them as older adults [26].
5.5. Accessibility of ICT
As highlighted in the study [20], reliable internet access is a crucial factor, and there are a large number of variations of ICT infrastructures in different parts of the world. Stable access to technology has sometimes been neglected in eHealth design for older adults [23, 52]. When the underlying infrastructure that is taken for granted is missing, services can entirely fail. In many countries, this can be a barrier to solutions that have been successful in other parts of the world. Countries with low-income populations often have an internal digital division that demands specific design solutions to address technological obstacles [37]. Finally, as highlighted in the study [34], eHealth systems for older adults should preferably have a simple and user-friendly technical design and have a straightforward focus on demonstrating the valuable benefits.
6. Conclusion
This study shed light on the major determinants of acceptance and adoption of eHealth systems for older adults. Trust in technology and personal ability to use the eHealth systems, personal integrity and privacy, fear to use new technology, eHealth education and literacy, and accessibility of ICT infrastructure and services are of utmost importance.
Findings also highlighted that independent living and human well-being should be the overall aim of future eHealth, which also was a recommendation in the study by [45]. In order to accomplish this aim, the suggestion is, as highlighted in the studies [22] and [25], a human-centred eHealth design, where the older adults should be actively involved, and empowered in the design and development of eHealth systems and services. Finally, proper education and training on the use of eHealth services is also of great importance.
7. Future Work
This study shed light on the main critical factors for human-computer interaction in the area of eHealth services for older adults. The interesting next step would be to investigate in which sub-fields older adults have the largest need for eHealth services and telecare. Further research is needed to investigate if the identified factors are general for all diseases, or how might their significance be changed depending on different types of diseases?
Acknowledgement
We would like to thank Pär-Ove Forss, Head of the Computer and System Science Department at Mid Sweden University, for his kind support throughout this research process.
Conflict of Interest
The authors declare no conflict of interest.
- M. Tonelli and M. Riella, “Chronic kidney disease and the aging population,” Brazilian Journal of Nephrology, vol.36, pp.1–5, 2014.
- F. P. Tajudeen, N. Bahar, T. Maw Pin, and N. I. Saedon, “Mobile technologies and healthy ageing: A bibliometric analysis on publication trends and knowledge structure of mHealth research for older adults,” International Journal of Human–Computer Interaction, vol.38, no. 2, pp.118–130, 2022.
- K. A. Kline and D. M. Bowdish, “Infection in an aging population,” Current opinion in microbiology, vol.29, pp.63–67, 2016.
- N. Stroetmann, T. Hüsing, L. Kubitschke, and K. A. Stroetmann, “The attitudes, expectations and needs of elderly people in relation to e-health applications: results from a European survey,” Journal of Telemedicine and Telecare, vol.8, no. 2_suppl, pp.82–84, 2002.
- L. Foster and A. Walker, “Active and successful aging: A European policy perspective,” The gerontologist, vol.55, no. 1, pp.83–90, 2015.
- C. Botella, E. Etchemendy, D. Castilla, R. M. Baños, A. García-Palacios, S. Quero, M. Alcaniz, and J. A. Lozano, “An e-health system for the elderly (Butler Project): A pilot study on acceptance and satisfaction,” CyberPsychology & Behavior, vol.12, no. 3, pp.255–262, 2009.
- A. Ahmad and P. Mozelius, “Critical factors for human computer interaction of ehealth for older adults,” Proceedings of the 2019 the 5th International Conference on e-Society, e-Learning and e-Technologies, pp.58–62, 2019.
- E. A. Phelan, L. A. Anderson, A. Z. Lacroix, and E. B. Larson, “Older adults’ views of ‘successful aging’—how do they compare with researchers’ definitions?,” Journal of the American Geriatrics Society, vol.52, no. 2, pp.211–216, 2004.
- A. Fiske, J. L. Wetherell, and M. Gatz, “Depression in older adults,” Annual review of clinical psychology, vol.5, pp.363–389, 2009.
- E. Y. Cornwell and L. J. Waite, “Social disconnectedness, perceived isolation, and health among older adults,” Journal of health and social behavior, vol.50, no. 1, pp.31–48, 2009.
- C. Christophorou, S. Kleanthous, D. Georgiadis, D. M. Cereghetti, P. Andreou, C. Wings, E. Christodoulou, and G. Samaras, “ICT services for active ageing and independent living: identification and assessment,” Healthcare technology letters, vol.3, no. 3, pp.159–164, 2016.
- S. T. Peek, K. G. Luijkx, M. D. Rijnaard, M. E. Nieboer, C. S. van der Voort, S. Aarts, J. van Hoof, H. J. Vrijhoef, and E. J. Wouters, “Older adults’ reasons for using technology while aging in place,” Gerontology, vol.62, no. 2, pp.226–237, 2016.
- S. Wiklund Axelsson and A. Melander Wikman, “Ready for eHealth. Older Swedes’ perceptions of eHealth Services: Using the PIADS scale as a predictor for readiness,” Technologies, vol.4, no. 3, p.29, 2016.
- C. Robert, M. Erdt, J. Lee, Y. Cao, N. B. Naharudin, and Y.-L. Theng, “Effectiveness of eHealth nutritional interventions for middle-aged and older adults: Systematic review and meta-analysis,” Journal of medical Internet research, vol.23, no. 5, p.e15649, 2021.
- L. A. Machi and B. T. McEvoy, “The literature review: Six steps to success (Third),” SAGE Publications, Inc, 2016.
- J. vom Brocke, A. Simons, B. Niehaves, B. Niehaves, K. Reimer, R. Plattfaut, and A. Cleven, “Reconstructing the giant: On the importance of rigour in documenting the literature search process,” 2009.
- V. Braun and V. Clarke, “Using thematic analysis in psychology,” Qualitative research in psychology, vol.3, no. 2, pp.77–101, 2006.
- V. Braun and V. Clarke, “Thematic analysis.,” 2012.
- O. B. Henkemans, K. E. Caine, W. A. Rogers, A. D. Fisk, M. A. Neerincx, and B. D. Ruyter, “Medical monitoring for independent living: user-centered design of smart home technologies for older adults,” Proc. Med-e-Tel Conf. eHealth, Telemedicine and Health Information and Communication Technologies, pp.18–20, 2007.
- M.L. Jung and K. Loria, “Acceptance of Swedish e-health services,” Journal of multidisciplinary healthcare, vol.3, p.55, 2010.
- W. A. Rogers and A. D. Fisk, “Toward a psychological science of advanced technology design for older adults,” Journals of Gerontology Series B: Psychological Sciences and Social Sciences, vol.65, no. 6, pp.645–653, 2010.
- E. Stojmenova, B. Imperl, T. Zohar, and D. Dinevski, “User-Centred E-Health: Engaging Users into the e-Health Design Process.,” Bled eConference, p.38, 2012.
- C. Lee and J. F. Coughlin, “PERSPECTIVE: Older adults’ adoption of technology: an integrated approach to identifying determinants and barriers,” Journal of Product Innovation Management, vol.32, no. 5, pp.747–759, 2015.
- S. H. Fischer, D. David, B. H. Crotty, M. Dierks, and C. Safran, “Acceptance and use of health information technology by community-dwelling elders,” International journal of medical informatics, vol.83, no. 9, pp.624–635, 2014.
- J. Vines, G. Pritchard, P. Wright, P. Olivier, and K. Brittain, “An age-old problem: Examining the discourses of ageing in HCI and strategies for future research,” ACM Transactions on Computer-Human Interaction (TOCHI), vol.22, no. 1, pp.1–27, 2015.
- A. J. De Veer, J. M. Peeters, A. E. Brabers, F. G. Schellevis, J. J. J. Rademakers, and A. L. Francke, “Determinants of the intention to use e-Health by community dwelling older people,” BMC health services research, vol.15, no. 1, pp.1–9, 2015.
- A. Ahmad, K. Ahlin, and P. Mozelius, “Technology Acceptance of an Online Speech and Language Assessment Application for Stroke Patients-the Medical Caregivers’ Viewpoints,” Tenth International Conference on Global Health Challenges (GLOBAL HEALTH 2021), Barcelona, Spain, October 3-7, 2021., 2021.
- Q. Ma, A. H. Chan, and P.-L. Teh, “Insights into older adults’ technology acceptance through meta-analysis,” International Journal of Human–Computer Interaction, vol.37, no. 11, pp.1049–1062, 2021.
- W. K. Bong and I. Bronshtein, “Designing Digital Games with & for Home-dwelling Older Adults’ Social Interaction under Sheltering Measures,” 2021.
- C. for D. Control and Prevention, “Improving health literacy for older adults: Expert panel report 2009,” Atlanta, GA: US Department of Health and Human Services, 2009.
- K. L. Courtney, G. Demeris, M. Rantz, and M. Skubic, “Needing smart home technologies: the perspectives of older adults in continuing care retirement communities.,” 2008.
- N. Charness and W. R. Boot, “Aging and information technology use: Potential and barriers,” Current Directions in Psychological Science, vol.18, no. 5, pp.253–258, 2009.
- N. Wagner, K. Hassanein, and M. Head, “Computer use by older adults: A multi-disciplinary review,” Computers in human behavior, vol.26, no. 5, pp.870–882, 2010.
- T. Heart and E. Kalderon, “Older adults: are they ready to adopt health-related ICT?,” International journal of medical informatics, vol.82, no. 11, pp.e209–e231, 2013.
- B. Xie, T. Yeh, G. Walsh, I. Watkins, and M. Huang, “Co-designing an e-health tutorial for older adults,” in Proceedings of the 2012 iConference, 2012, pp.240–247.
- R. Young, E. Willis, G. Cameron, and M. Geana, “‘Willing but unwilling’: attitudinal barriers to adoption of home-based health information technology among older adults,” Health informatics journal, vol.20, no. 2, pp.127–135, 2014.
- C. Latulipe, A. Gatto, H. T. Nguyen, D. P. Miller, S. A. Quandt, A. G. Bertoni, A. Smith, and T. A. Arcury, “Design considerations for patient portal adoption by low-income, older adults,” Proceedings of the 33rd annual ACM conference on human factors in computing systems, pp.3859–3868, 2015.
- A. Bowes and G. McColgan, “Telecare for older people: promoting independence, participation, and identity,” Research on Aging, vol.35, no. 1, pp.32–49, 2013.
- A. Melander-Wikman, Y. Fältholm, and G. Gard, “Safety vs. privacy: elderly persons’ experiences of a mobile safety alarm,” Health & social care in the community, vol.16, no. 4, pp.337–346, 2008.
- Y. van Hierden, T. Dietrich, and S. Rundle-Thiele, “Designing an eHealth Well-Being Program: A Participatory Design Approach,” International Journal of Environmental Research and Public Health, vol.18, no. 14, p.7250, 2021.
- M. Jovanović, A. De Angeli, A. McNeill, and L. Coventry, “User requirements for inclusive technology for older adults,” International Journal of Human–Computer Interaction, vol.37, no. 20, pp.1947–1965, 2021.
- T. Wang, S. R. Mazanec, and J. G. Voss, “Needs of Informal Caregivers of Patients With Head and Neck Cancer: A Systematic Review,” Oncology Nursing Forum, vol.48, no. 1, pp.11–29, 2021.
- Z. Zhou, J. Zhou, and F. Liu, “Fewer Steps the Better? Instructing Older Adults’ Learning and Searching in Smartphone Apps,” International Journal of Human–Computer Interaction, pp.1–12, 2021.
- M. N. Hossain, H. Okajima, H. Kitaoka, and A. Ahmed, “Consumer acceptance of eHealth among rural inhabitants in developing countries (A Study on Portable Health Clinic in Bangladesh),” Procedia computer science, vol.111, pp.471–478, 2017.
- L. T. Vassli and B. A. Farshchian, “Acceptance of health-related ICT among elderly people living in the community: A systematic review of qualitative evidence,” International Journal of Human–Computer Interaction, vol.34, no. 2, pp.99–116, 2018.
- N. Bhatnagar, H. Madden, and Y. Levy, “Initial empirical testing of potential factors contributing to patient use of secure medical teleconferencing,” Journal of Computer Information Systems, vol.57, no. 1, pp.89–95, 2017.
- N. Davis, K. Shiroma, B. Xie, T. Yeh, X. Han, and A. De Main, “Designing eHealth tutorials with and for older adults,” Proceedings of the Association for Information Science and Technology, vol.58, no. 1, pp.92–103, 2021.
- R. Verma, C. Saldanha, U. Ellis, S. Sattar, and K. R. Haase, “eHealth literacy among older adults living with cancer and their caregivers: A scoping review,” Journal of Geriatric Oncology, 2021.
- K. Oberschmidt, C. Grünloh, F. Nijboer, and L. van Velsen, “Best Practices and Lessons Learned for Action Research in eHealth Design and Implementation: Literature Review,” Journal of Medical Internet Research, vol.24, no. 1, p.e31795, 2022.
- M. Thapliyal, N. J. Ahuja, A. Shankar, X. Cheng, and M. Kumar, “A differentiated learning environment in domain model for learning disabled learners,” Journal of Computing in Higher Education, pp.1–23, 2021.
- M. S. Wolf, J. A. Gazmararian, and D. W. Baker, “Health literacy and functional health status among older adults,” Archives of internal medicine, vol.165, no. 17, pp.1946–1952, 2005.
- C. Scheerens, J. Gilissen, A. M. Volow, J. L. Powell, C. M. Ferguson, D. Farrell, B. Li, C. Berry, and R. L. Sudore, “Developing eHealth tools for diverse older adults: Lessons learned from the PREPARE for Your Care Program,” Journal of the American Geriatrics Society, vol.69, no. 10, pp.2939–2949, 2021.
No related articles were found.
